Internal Emails Show How Chaos at the CDC Slowed the Early Response to Coronavirus
On Feb. 13, the U.S. Centers for Disease Control and Prevention sent out an email with what the author described as an “URGENT” call for help.
The agency was struggling with one of its most important duties: keeping track of Americans suspected of having the novel coronavirus. It had “an ongoing issue” with organizing — and sometimes flat-out losing — forms sent by local agencies about people thought to be infected. The email listed job postings for people who could track or retrieve this paperwork.
“Help needed urgently,” the CDC wrote.
This email is among hundreds of pages of correspondence between federal and state public health officials obtained by ProPublica through a records request in Nevada.
During the period in which the correspondence was written, from January to early March, health officials were trying to stay ahead of the coronavirus outbreak underway in China. By mid-February, when the CDC job postings email went out, the virus had a toehold in the United States, where there were already 15 confirmed cases. In another two weeks, the first case of community transmission would be reported in California, followed shortly by cases in Washington.
The documents — mostly emails — provide a behind-the-scenes peek into the messy early stages of the U.S. response to the coronavirus, revealing an antiquated public health system trying to adapt on the fly. What comes through clearly is confusion, as the CDC underestimated the threat from the virus and stumbled in communicating to local public health officials what should be done.
The same week the CDC sent out the email about the job openings, the agency sent Nevada officials alerts about 80 potential coronavirus patients to monitor, documents show. Four were not Nevada residents.
A state epidemiologist, in each instance, corrected the agency, informing the CDC that the person was from New York, not Nevada. (The CDC then redirected each report to New York, the documents show.)
The confusion sometimes went both ways. On March 4, a program manager in the Nevada Health Department reached out to the CDC to ask about congressional funding for COVID-19, the disease caused by the novel coronavirus.
“There seems to be a communications blackout on this end,” the program manager wrote, wondering if funds would be distributed based on the number of cases in each state or by population.
“Unfortunately, there is no clear answer to your questions,” responded a CDC staffer, apologizing for the lack of information. “We are hearing all of the rumor mills as well.”
“Thank you,” the Nevada program manager replied. “It’s good to be confused together.”
Chaotic Coordination
For much of February, the CDC kept a tight grip on who should be tested for the coronavirus, a strategy that has been criticized by epidemiologists for limiting the ability to track the spread of the disease.
In a Feb. 19 presentation to state health officials, the CDC described the definition of a person who ought to be tested: You had to have had close contact with someone confirmed to have COVID-19, or to have traveled from China and then had respiratory symptoms and a fever at the same time.
However, the CDC’s own guidance from a month prior, distributed to the states on Jan. 17, had a footnote that said that “fever may not be present in some patients,” such as people who had taken fever-lowering medications, according to one of the documents obtained by ProPublica. That caveat was not on the slides presented to the states in mid-February.
In a statement to ProPublica, the CDC said clinicians could always use their judgment to decide who received a test. “CDC never declined a request for testing that came from a state or local health department,” the agency said.
In mid to late February, the CDC was trying to move responsibility for coronavirus testing from itself to state health departments — a critical step, since the CDC does not have the capacity to be the nation’s testing lab. Slides from the Feb. 19 presentation describe the process for transitioning from “Phase 1,” in which the CDC determined who was a potential COVID-19 patient and conducted all the testing, to “Phase 2,” in which local health departments would do that work and report data back to the CDC.
Because of delays with test kits, Phase 2 had to be “redesigned,” the presentation said, so the CDC would continue to test specimens and return results. The CDC told ProPublica that all states have now transitioned to the original Phase 2 plan, where they can run their own tests.
The CDC presentation also directed the states to use a web platform called DCIPHER, which the agency was already using for food-related outbreaks, to report potential COVID-19 patients and confirmed cases.
But it wasn’t until the week of Feb. 24 — the same week that the U.S. would discover its first case of community-acquired COVID-19 — that the CDC scheduled a training for states on how to use the platform, according to the documents.
On March 1, the CDC emailed Nevada’s Health Department, requesting that it send a list of users and email addresses to connect to the DCIPHER system, to “ensure that we can onboard your jurisdiction.”
“We sent a spread sheet a couple weeks ago which I thought covered this,” a state epidemiologist responded.
Four days later, Nevada announced its first confirmed case of the coronavirus. It’s unclear when the state managed to successfully get on the DCIPHER system. Officials from Nevada declined to comment.
“Maybe Just Kidding”
A key part of the CDC’s strategy during the early days of the outbreak was identifying infected travelers returning from China. The process for screening passengers arriving at Los Angeles International Airport did not go smoothly, the correspondence obtained by ProPublica indicates.
On Feb. 16, a CDC staff member sent a message to colleagues about a buggy electronic traveler screening questionnaire that wouldn’t save correctly, among other issues. Also, the tool’s drop down field auto-populated with “United Kingdom” instead of “United States,” forcing users to type “United States of America.”
The CDC staffer also said the agency was struggling to interview non-English speakers in a timely manner and needed additional interpreters.
“Hello Team,” another CDC staff member responded, offering a solution: “The Google translate App has a real-time voice translation option.”
The screening protocol also wasn’t always clear. On Feb. 29, a CDC officer at LAX sent an email to her colleagues, saying: “In case this comes up again, we are not screening private flights. These would be flights that land at LAX but don’t arrive into the regular terminal … mainly for rich people.”
Just over two hours later, the officer emailed again. “And, maybe just kidding,” she wrote. Information from headquarters seemed to contradict what she had said about private flights, she said.
The CDC told ProPublica that it scaled up the screening almost overnight, so it focused on vetting the largest segment possible of high-risk passengers coming from places like Wuhan, China. The agency trained staff and dealt as best it could with limited staffing and translation services, it said.
“Protecting Americans Is What We Do”
The CDC’s initial response to COVID-19, particularly its failure to initiate swift, widespread testing, has drawn intense criticism.
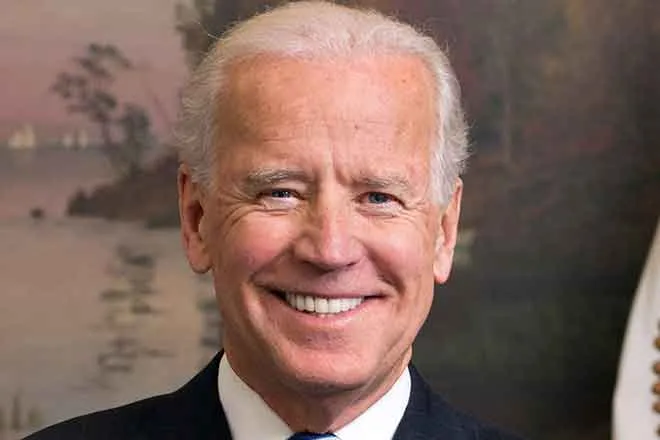
Nonetheless, the correspondence ProPublica obtained shows that the CDC director, Dr. Robert Redfield, exuded confidence in communications with others at the agency.
On Jan. 28, when the CDC had confirmed five cases of the coronavirus, all in travelers who arrived from outside the country, he emailed colleagues to acknowledge it posed “a very serious public health threat,” but he assured them “the virus is not spreading in the U.S. at this time.”
That actually may not have been the case. The CDC confirmed the first case of COVID-19 in Washington on Jan 20. Trevor Bedford, a computational epidemiologist at the Fred Hutchinson Cancer Research Center in Seattle, has said he believes that the virus could have begun circulating in the state immediately after the traveler arrived in mid-January, based on his analysis of genetic data from the initial Washington cases.
The CDC said in its statement that Redfield’s comments were based on the data available at the time. “At no time, did he underestimate the potential for COVID-19 becoming a global pandemic,” the agency’s statement said. “He stated consistently that more cases, including person to person spread, were likely.”
On March 3, Redfield wrote to his staff again, stressing the agency’s readiness, despite the growing evidence that it wasn’t. “We anticipated and prepared for the possible spread of COVID-19 in communities across the United States,” he said in an email.
The CDC said in its statement that Redfield was telling staffers that the agency would continue to be engaged in a sustained response to COVID-19. Redfield’s email was not characterizing the state of the outbreak, the CDC said.
By that point, it was clear that the coronavirus was gaining ground within the country, even if the inability to test for it was obscuring the true numbers. Physicians and public health experts begged for more tests while warning that thousands of cases would soon emerge.
Still, Redfield’s March 3 email struck a reassuring note.
“Confronting global outbreaks and protecting Americans is what we do,” Redfield wrote in the message. “More and more, people are turning to us for guidance, and we respond consistently with evidence-based information and professionalism.”