Cell-like decoys could mop up viruses in humans – including the one that causes COVID-19

Liangfang Zhang, University of California San Diego
The Research Brief is a short take about interesting academic work.
The big idea
Researchers around the world are working frantically to develop COVID-19 vaccines meant to target and attack the SARS-CoV-2 virus. Researchers in my nanoengineering lab are taking a different approach toward stopping SARS-CoV-2. Instead of playing offense and stimulating the immune system to attack the SARS-CoV-2 virus, we’re playing defense. We’re working to shield the healthy human cells the virus invades.
Conceptually, the strategy is simple. We create decoys that look like the human cells the SARS-CoV-2 virus invades. So far, we’ve made lung-cell decoys and immune-cell decoys. These cell decoys attract and neutralize the SARS-CoV-2 virus, leaving the real lung or immune cells healthy.
To make the decoys, we collect the outer membranes of the lung or immune cells and wrap them around a core made of biodegradable nanoparticles. From the outside the decoys look the same as the human cells they are impersonating. Our decoys are hundreds of times smaller in diameter than an actual lung or immune cell, but they have all the same cellular hardware sticking out of them.
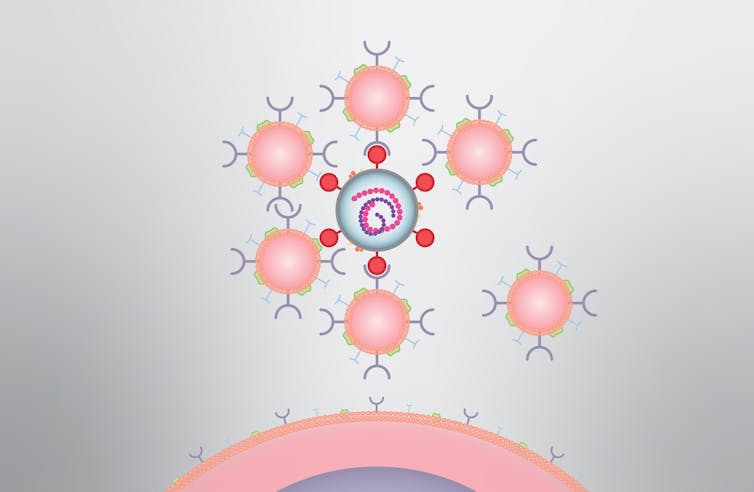
We call them “nanosponges” because they soak up harmful pathogens and toxins that attack the cells they impersonate. My team and I first developed the concept 10 years ago, and since then we’ve shown the nanosponges offer a new approach to fighting viral infections like HIV; bacterial infections like methicillin-resistant Staphylococcus aureus, or MRSA, E. coli and sepsis; and inflammatory diseases like rheumatoid arthritis.
We recently published results showing that the SARS-CoV-2 coronavirus binds to these decoy nanosponges, which were more than 90% effective in causing the virus to lose its ability to infect cells in petri dishes. Once the virus is locked into the decoy, it can’t invade any real cells, and is cleared by the body’s immune system.
Why it matters
Vaccines are critical for protecting against viral infections, but as viruses mutate they can render vaccines and treatments ineffective. This is why new flu vaccines are developed each year. Fortunately, SARS-CoV-2 doesn’t appear to mutate as quickly as influenza viruses, but this highlights the need for alternatives that are unaffected by mutations.
I’m hopeful that other teams of researchers come up with safe and effective treatments for COVID-19 as soon as possible. But for now, my team is working and planning as if the world is counting on us.
What still isn’t known
The different types of nanosponges we’ve developed are in various stages of pre-clinical development. So far, the results look promising, but there is more work to do to ensure they’re safe and effective.
Cellular nanosponges are a new kind of drug. We made the first nanosponges using human red blood cell membranes, and these are the furthest along in the regulatory process, having undergone all stages of pre-clinical testing.
What’s next
Cellics Therapeutics, a startup company I co-founded, is in the process of submitting an investigational new drug application to the FDA for the red blood cell nanosponges to treat bacterial pneumonia. If these red blood cell nanosponges get FDA approval and if the pre-clinical data for the COVID-19 nanosponges keep looking good, the COVID-19 nanosponges could have a clearer path to clinical trials in the years ahead.
We are currently testing the nanosponges for SARS-CoV-2 in animals. If the nanosponges do reach the clinical trial stage, there are several ways of delivering the therapy, including direct delivery into the lung for intubated patients via an inhaler like those used by asthmatic patients or through an intravenous injection.
There is also the possibility that our immune-cell nanosponges could soak up the inflammatory cytokine proteins that are triggering the dangerous immune system overreactions in some people suffering from COVID-19.
[You need to understand the coronavirus pandemic, and we can help. Read The Conversation’s newsletter.]![]()
Liangfang Zhang, Professor of Nanoengineering, University of California San Diego
This article is republished from The Conversation under a Creative Commons license. Read the original article.